So we have made it to this point. You have been rolling, stretching, warming up before your runs, but your nagging shin splint pain will not go away. Maybe it has improved 50%, but as you continue to train for your upcoming event, the pain has plateaued. Sound familiar?
Resolve Low Back Issues Part 4: Most Common Myths Of Low Back Pain
Few musculoskeletal conditions have a cult-like following of myths as Low Back Pain, many of which have been said by various healthcare providers across all specialties. To help clear the air, let's take a look at the 5 most common misunderstandings and myths that we encounter in our chiropractic clinic that could actually make your low back pain worse.
Runner's Knee Part 3: Training Modification & Self-Care
Over the last two weeks, we have discussed the ins and outs of what Patellofemoral Pain Syndrome is, the anatomy involved, how adjacent joints (hip and ankle) can lead to maltracking issues, and why runner’s are specifically susceptible to this common overuse injury. You can read Part 1 & Part 2 here.
Now it’s time to talk self-treatment and training modification. Our goal is to maintain training (load) if possible when you find Runner’s Knee settling in, but more times than not, rest and self-care is needed while also modifying our training volume and intensity until symptoms recede.
The Best Running Warm-Up To Help Prevent Injury
If you are like SOME runners, you prepare for your run by completing two quick stretches. First, you bend over and touch your toes. Next, you stand up, grab your foot from behind, and pull it toward your butt.
If you are like MOST runners, you don't even do that! In place of a long-winded stance on why you should be doing this and how research shows that warming-up before exercise not only prevents injury but improves performance. We are going to cover the bases of a great running warm-up through our Bands, Balance, & Bounce Running Warm-Up Routine.
How 'The Big 3' Can Decrease Low Back Pain and Make You Stronger & Faster
If you are among the estimated 50% of all athletes who experience recurrent low back pain, don’t stress, there are exercises that can help…and a couple you should probably avoid.
Our ‘core’ is the link between our upper and lower bodies, and mastery of control here is the secret to improved strength, running efficiency, faster speed, and overall health and athleticism. In regards to back pain, our core needs to be solid to not only support a stable spine but provide for proper biomechanics when running, throwing, squatting, swimming, and even just walking.
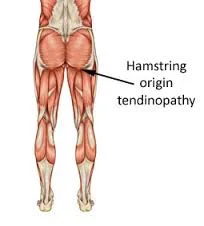
Hamstring: Proximal Strain & Tendinopathy
Hamstring injuries can be a beast; they drag you down mentally and physically as treatment tends to draw out and disrupt your training plans and goals. They present with pain and tenderness near the gluteal fold and over the posterior thigh, making it sometimes difficult to run, ride, walk and even sit. What I would like to do here today is briefly (as a longer post is to come later) give you some basic suggestions based on research findings, what patients have responded positively to, as well as what to do about your training and overall fitness.